You may have experienced low back pain (LBP) years ago, but this time around it’s different—simply because you’re older. For one thing, it’s more common.
Geriatric back pain leads the list of musculoskeletal disabilities for older adults throughout the world, partly because aging alone can affect all of your body systems. But it’s not only the causes that vary; the impact of LBP also changes as you age.
LBP culprits
While low back pain affects all ages, young people may be able to identify temporary reasons for the condition, such as pregnancy, toting a heavy backpack or even just poor posture. For adults, a review of the recent literature on low back pain identifies four risk factors:
- Workplace demands. Heavy lifting, pushing and pulling, driving a vehicle and prolonged walking or standing all have an association with low back pain. Psychological factors surrounding work—stress, dissatisfaction, monotony—also contribute to back pain. This is why socioeconomic studies show that low back pain is less prevalent among people who work in professional, managerial or other positions that require less physical demand.
- Obesity. LBP correlates with higher body mass index.
- Over- or under-exercising. People who exercise one to five times a week report less low back pain than people who work out either more frequently or less frequently. The current recommendation for adults is to participate in 150 minutes of moderate activity a week.
- Being female. Many studies have found that postmenopausal women report more, or more severe, low back pain than men of the same age. However, some research suggests that men simply are less likely to report the pain or rate it as severe.
What’s going on back there?
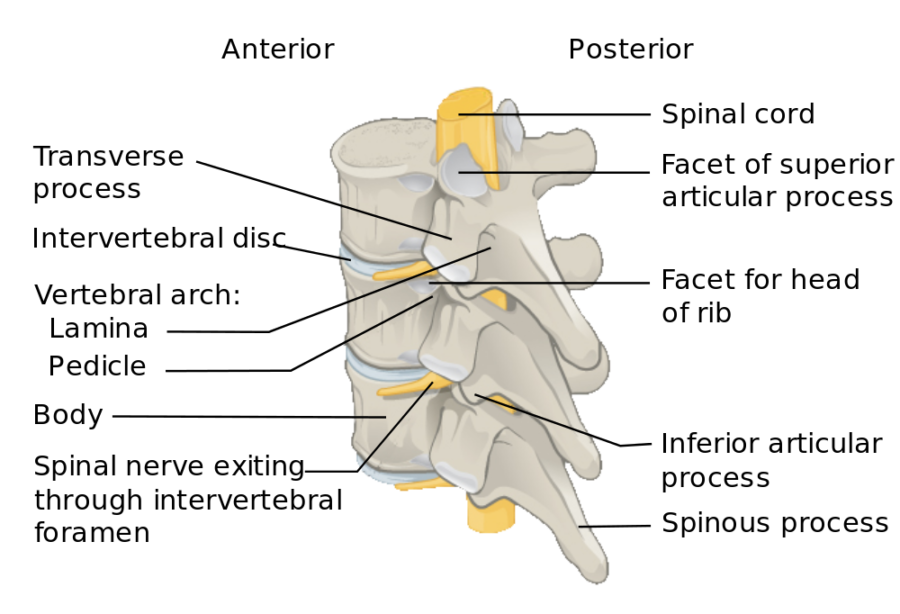
The 24 bones, or vertebrae, that make up the spinal column encase the spinal cord from the skull to the tailbone. Linked by little joints called facets, the bones rest on cushion-like discs that fill the space between each two vertebrae. Three major ligaments help to stabilize the spine.
All day long as you sit, stand, bend and lie down, your spine must adjust to each changing position. With so many moving parts, eventually things are bound to wear out, dislodge and otherwise just go wrong. “Spondylosis” is the term for this normal wear and tear, while “sarcopenia” refers to age-related loss of muscle mass and function. Three of the most common lower back deterioration issues after age 50 are:
- Degenerative changes in discs and joints. Discs, especially, are meant to be shock-absorbers, but over time they can become less effective as they lose moisture and resilience.
- Spinal stenosis. This condition refers to a narrowing of the spaces within the spine. It happens when the ligaments thicken, discs degenerate or arthritis attacks the facet joints. In addition to the lower back, the neck area can take a hit from this.
- Spondylolisthesis. Most likely to occur at the base of the spine, a defect or fracture in a vertebra causes it to slip onto the vertebra below.
Of course, back pain also can be tied to injuries, tumors, kidney stones and other factors that can come into play at any time in someone’s life. Underlying conditions such as osteoporosis, arthritis, endometriosis and fibromyalgia can impact the spine as well. As with any part of the body, nerves can get damaged and cause pain or numbness.
LBP’s heavy impact
Older adults with low back pain suffer more than just physical pain; they pay a psychological and cognitive price as well. Studies of older adults suggest that chronic back pain can lead to:
- Depression
- A loss of confidence in functional capacity
- A decline in memory
- Diminished executive function
- Decreased walking speed
In short, people in chronic pain seem to age faster than their peers.
LBP treatment
A condition with as many causes and consequences as low back pain requires a comprehensive examination to determine what to do about it. Treatment ranges from surgery, steroids and nerve blocks to acupuncture, over-the-counter anti-inflammatory medication and simple rest and hot/cold application. Physical therapy is another popular option.
“Geriatric low back pain should be addressed as aggressively as low back pain for younger people,” says physical therapist Patrick Donovan, owner of Heather Lane Physical Therapy in Denver. “Although aging often contributes to the cause, aging should not be used as an excuse for lighter treatment. We always aim to decrease pain intensity and pain with movement while increasing physical activity levels and physical function—no matter what the person’s age.”
Citations
Leboeuf-Yde, Kyvik KO (1998). At what age does low back pain become a common problem? A study of 29,424 individuals aged 12-41 years. Spine (Phila Pa 1976). 1998 Jan 15; 23(2): 228-34.
DePalma, Michael J., Ketchum, Jessica M., and Saullo, Thomas. What Is the Source of Chronic Low Back Pain and Does Age Play a Role? Pain Medicine (Volume 12, Issue 2). Feb. 2011: 224–233. https://doi.org/10.1111/j.1526-4637.2010.01045.

