I’m Over 60—is Urinary Incontinence Normal?
When you’re pregnant and experience urinary leaking, the cause is obvious, and you figure that everything concerning your health will go back to normal once the baby is out and no longer pressing on your bladder. Typically, that’s exactly what happens. But years later urinary incontinence (UI) can show up again—and this time there’s no baby to blame. You don’t want to stop drinking water or resort to wearing Depends. So what should you do?

Although men and women of any age can experience urinary incontinence, reports show the highest incidence of UI occurring in women over 60. The University of Pittsburgh Schools of the Health Sciences estimates that three times as many women as men experience urinary incontinence and that only 1 in 12 people suffering from UI seek help.
“Many women accept pelvic health disorders as a normal part of aging and don’t seek treatment,” agrees Dr. Brett Vassallo, a urogynecologist at Advocate Lutheran General Hospital in Park Ridge, Illinois. “There is no reason to suffer in silence or feel embarrassed speaking to your doctor. Pelvic health disorders are treatable and often curable.”
Diagnosing UI
The average bladder can hold 10-17 fluid ounces, but the urge for urination occurs when the bladder is only about one-quarter full. Diagnosis normally begins with a questionnaire that asks the patient:
- How often do you leak?
- How much urine leaks?
- How much does leakage interfere with your everyday life?
- Under what conditions does this occur—before you can get to the toilet, when you cough or sneeze, when you’re asleep, when you’re physically active or exercising, after you’ve urinated and gotten dressed again or for no obvious reason?
Additionally, a doctor may conduct a physical exam and do a bladder stress test. The patient may also be asked to keep a bladder diary for a few days.
According to the American College of Obstetricians and Gynecologists (ACOG), the diagnosis for this condition will fall into one of three categories:
- Stress urinary incontinence (SUI), characterized by leaking urine when coughing, laughing, sneezing, exercising or even just walking.
- Urgency urinary incontinence, a sudden, strong urge to urinate that is hard to hold back; signs include leaking urine on the way to the bathroom. People with an overactive bladder (OAB)—33 million men and women in the U.S., according to the American Urological Association—have this diagnosis.
- Mixed incontinence, which combines symptoms of both SUI and urgency urinary incontinence.
How does this happen?
A comprehensive exam will identify the cause for the condition. Causes include:
- Urinary tract infection (UTI).
- Diuretic medications, caffeine or alcohol—all substances that cause the body to generate more urine.
- Constipation, which often accompanies urinary incontinence, especially in older women.
- Neuromuscular problems that occur when the brain’s normal signals to the bladder and urethra are disrupted.
- Anatomical problems that can occur when bladder stones or other growths block the outlet of the bladder into the urethra.
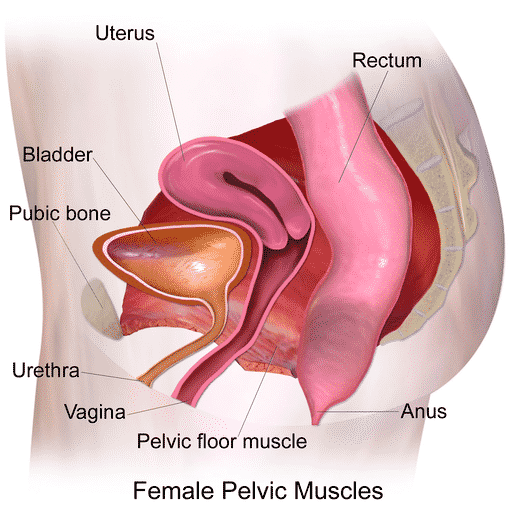
- Pelvic floor disorders (PFD) caused by a weakening of the muscles, ligaments and connective tissues in the lowest part of the pelvis. In addition to urinary incontinence, these disorders can cause bowel leakage and pelvic organ prolapse.
- Diseases like diabetes, Parkinson’s and multiple sclerosis, which can damage the nerves that control the bladder. Infections, strokes, surgeries, Alzheimer’s and treatments for pelvic cancers also can impact the urinary function.
Because doctors tend to recommend trying the least invasive solutions first, physical therapy often comes into play early with urinary incontinence. Studies increasingly show that physical therapy can benefit patients with all categories of UI, according to physical therapist Dr. Patrick Donovan at Heather Lane Physical Therapy. In a future article, we’ll review physical therapy approaches and other solutions for patients diagnosed with urinary incontinence.
Citation:
https://www.urologyhealth.org/urologic-conditions/urinary-incontinence
https://jamanetwork.com/journals/jama/article-abstract/271857
https://uroweb.org/wp-content/uploads/Urinary-Incontinence-2010.pd
The information provided on this site is intended for your general knowledge only and is not a substitute for professional medical advice or treatment for specific medical conditions. You should not use this information to diagnose or treat a health problem or disease without consulting with Heather Lane Physical Therapy or another qualified healthcare provider.