If you’re one of the more than 250 million people suffering with osteoarthritis (OA), you probably struggle with pain and decreased mobility. And if you’re not, you may want to take preventive measures to avoid joining the roughly 10 percent of men and 13 percent of women over the age of 60 who have osteoarthritis of the knee—a key joint for so many everyday movements.
Symptoms of osteoarthritis of the knee
Pain is the hallmark symptom of osteoarthritis of the knee as well as of other joints. Sufferers often experience “pain flares”—short episodes of intense and unpredictable pain. As a result, people with arthritis of the knee may shy away from participating in social or physical activity to avoid triggering a flare.
4 progressive stages of osteoarthritis of the knee
Osteoarthritis of the knee is a progressive disease with four stages:
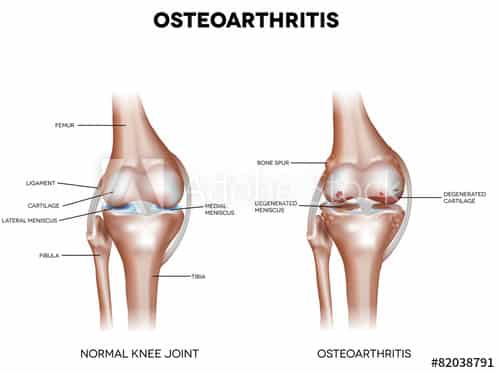
Stage 1: Minor. The patient isn’t experiencing pain, and even the X-ray may appear normal. But bone spurs—small lumps of bone called “osteophytes“—are starting to form where bone meets bone.
Stage 2: Mild. Some stiffness or joint pain is noticeable as osteophyte growth increases, the cartilage begins to thin, a layer of bone develops in the joints beneath the cartilage, and the area where the bones and tissues meet starts to harden, making the bone thicker and denser. At this stage, the joint’s synovial fluid is still keeping the bones from scraping against each other.
Stage 3: Moderate. The patient is uncomfortable no matter what. Sitting results in stiffness, while walking, kneeling and bending trigger pain from joint inflammation. The cartilage is further thinning and breaking down, narrowing the space between the bones and causing the bones to thicken and form lumps.
Stage 4: Severe. At this most advanced level, the cartilage is almost completely gone, the synovial fluid is significantly reduced and the space between the bones has further narrowed. The knee joint may feel stiff or immobile and also appear deformed. This is the “bone-on-bone” stage, when patients typically suffer great pain with any movement of the knee.
Preventing osteoarthritis of the knee
Physical inactivity significantly contributes to osteoarthritis of the knee, so the best prevention is a tailored exercise program to maintain flexibility and strength around the knee and joints. A physical therapist can design a program to help aging adults preserve motion and cartilage in the knee, maintain knee health and retain independence. Weight loss may be recommended to decrease excessive stress on the joint and minimize pain flares.
Stopping or slowing progression
Despite a common misconception that physical activity makes osteoarthritis of the knee advance or further damage the joints, studies show that supervised exercise therapy helps to decrease activity-related pain in patients. Sufferers from arthritis of the knee who maintain higher activity levels have fewer severe pain flares, which helps them get through daily life without discomfort.
The converse is true as well: restricting physical activity risks making knee OA worse.
To assess your physical fitness and ability to perform routine activities, your physical therapist may ask you to undergo the 30-second chair-stand test. This test measures how many times within a 30-second period you can get up from sitting on a chair.
Is arthritis of the knee reversible or curable?
You can’t reverse existing knee damage from osteoarthritis. At Stage 4, surgery is typically recommended and may include a full knee replacement. In earlier stages, the condition is treated with increasingly aggressive levels of medication.
Physical activity is your best bet. At Stages 1-3, physical activity substantially decreases the risk of functional decline—the inability to do routine activities like bathing and dressing—for people with osteoarthritis of the knee, as well as at least 34 other chronic conditions.
Exercises that help to prevent and relieve pain from knee OA
Your PT will customize a home exercise program for you depending on your specific needs. View two exercises here that can strengthen your outside hip and reduce pain.
The majority of patients with pain in the front part of their knee have weak quadriceps (thigh muscles). Within that muscle group, many people with knee pain also have an underdeveloped vastus medialis, a muscle that extends from the inner thigh to the inner knee. These are the most critical muscles to strengthen for people with osteoarthritis of the knee seeking non-surgical alternatives.
Also, strengthening the whole leg and outside hip may reduce knee pain and help knee OA sufferers return to normal activities. Your physical therapist can design a multi-phase program that fortifies your legs and prepares your body for doing daily tasks with less struggle and pain.
Call Heatherlane Physical Therapy at (720) 507-3962 or book an appointment online today for your personalized osteoarthritis of the knee action plan and pain-reduction program.
Photo by Anna Auza on Unsplash
Diagram by Adobe Photos
Citations:
Anterior Knee Pain: What Muscles Should I Strengthen? (2018). Journal of Orthopaedic & Sports Physical Therapy, 48(1), 32–32. doi: 10.2519/jospt.2018.0501
Skou, S. T., Grønne, D. T., & Roos, E. M. (2019). Prevalence, Severity, and Correlates of Pain Flares in Response to a Repeated Sit to Stand Activity: A Cross-Sectional Study of 14,902 Patients With Knee and Hip Osteoarthritis in Primary Care. Journal of Orthopaedic & Sports Physical Therapy, 1–26. doi:
10.2519/jospt.2019.9125
Werner, S. (2014). Anterior knee pain: an update of physical therapy. Knee Surgery, Sports Traumatology, Arthroscopy, 22(10), 2286–2294. doi: 10.1007/s00167-014-3150-y
Zhang, Y., & Jordan, J. M. (2010). Epidemiology of Osteoarthritis. Clinics in Geriatric Medicine, 26(3), 355–369. doi: 10.1016/j.cger.2010.03.001

